In the realm of medical breakthroughs, the introduction of the first drug designed to slow the progression of Alzheimer’s disease marked a significant milestone over a year ago.
However, despite its potential to revolutionize treatment for this debilitating condition, sales of the drug, Leqembi, have not met initial expectations.
Major hospital systems have encountered delays in incorporating it into their treatment protocols, and some insurers have been hesitant to provide coverage for this innovative medication.
Physicians are expressing concerns about patient reluctance to embrace Leqembi due to its limited efficacy and potential side effects. They emphasize the need for extensive research to optimize the drug’s utilization and stress the importance of enhancing diagnostic procedures in the field of Alzheimer’s disease.
Dr. Ambar Kulshreshtha, a dedicated family physician specializing in dementia patients in suburban Atlanta, underscores the commencement of a promising yet challenging journey with the introduction of Leqembi.
With over 6 million Americans and countless individuals worldwide affected by Alzheimer’s disease, the urgent need for effective treatments is undeniable.
While Leqembi targets the accumulation of amyloid protein in the brain, a hallmark of Alzheimer’s, its impact is modest, with studies suggesting a mere delay in disease progression for individuals with mild symptoms.
Some experts question whether this delay is perceptible enough for patients to discern any tangible benefits.

Moreover, the potential adverse effects of Leqembi, such as brain swelling and bleeding, necessitate regular monitoring through brain scans.
The drug received full approval from the Food and Drug Administration for early-stage Alzheimer’s patients, with coverage under the federal Medicare program for individuals aged 65 and above.
However, the cost implications of the drug, coupled with the expenses associated with diagnostic scans, pose financial challenges for patients, given Leqembi’s annual price exceeding $26,000.
Eisai, the pharmaceutical company behind Leqembi, initially anticipated a substantial uptake of the drug, aiming for 10,000 patients receiving treatment by March. However, logistical hurdles have impeded the swift adoption of Leqembi within healthcare systems.
Alexander Scott, an executive at Eisai, acknowledges the intricate process of integrating a novel drug like Leqembi into existing healthcare frameworks, requiring substantial time and resources.
Health systems across the United States have embarked on a gradual rollout of Leqembi, with institutions like Cedars-Sinai in Los Angeles and Banner Health in Arizona introducing the drug in specialized clinics after meticulous planning and coordination.
The Mayo Clinic in Minnesota has restricted Leqembi administration to patients within a 100-mile radius to ensure swift response to any adverse reactions, underscoring the cautious approach adopted by healthcare providers.
As healthcare facilities navigate the complexities of drug coverage, infusion protocols, and diagnostic procedures associated with Leqembi, the challenge lies in ensuring that patients receive comprehensive care without facing financial burdens.
The evolving landscape of insurance coverage for the drug remains a pivotal factor influencing patient access and adherence to treatment regimens.
In conclusion, the sluggish uptake of Leqembi underscores the multifaceted challenges inherent in introducing innovative therapies for complex conditions like Alzheimer’s disease.
While the road ahead may be fraught with obstacles, the collaborative efforts of healthcare providers, pharmaceutical companies, insurers, and policymakers are crucial in maximizing the potential benefits of Leqembi and advancing the field of Alzheimer’s treatment.
The journey towards combating Alzheimer’s disease is indeed a complex and arduous one, demanding sustained commitment and collaboration from all stakeholders involved.
In the realm of healthcare, the accessibility of treatments for Alzheimer’s disease remains a poignant concern, particularly for patients who do not meet the criteria for Medicare coverage due to their age.
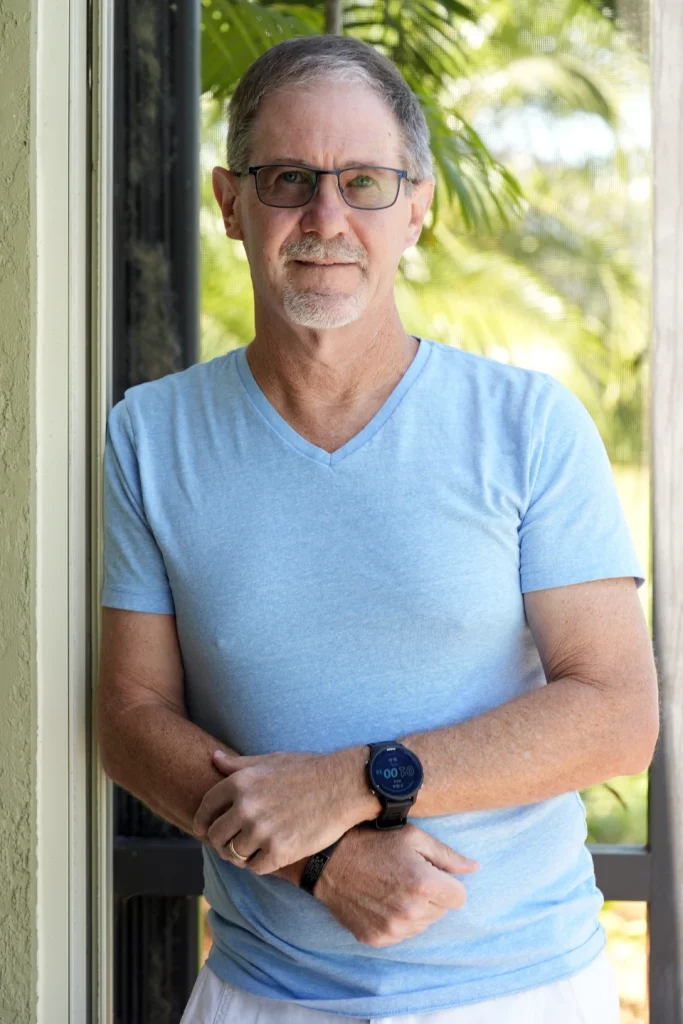
The narrative of Scott Berkheiser from Venice, Florida, sheds light on the hurdles faced by individuals seeking timely medical interventions.
Despite being eligible for Leqembi infusion, insurance denials impeded Berkheiser’s treatment initiation, leading to a delay until last December. This scenario underscores the intricate web of challenges that patients encounter in navigating the healthcare system.
The ordeal faced by Berkheiser is not an isolated incident. Texas Neurology’s experience with Leqembi reveals the complexities surrounding treatment commencement.
Despite having 60 potential candidates on a waitlist, only a fraction were able to initiate treatment. The constraints of time and disease progression create a sense of urgency in identifying suitable patients and commencing treatment promptly.
The poignant remark by CEO David Evans on the fleeting window of opportunity underscores the critical need for streamlined processes in healthcare delivery.
Moreover, the diagnostic journey for Alzheimer’s disease presents its own set of challenges. The intricate process of ruling out reversible causes before proceeding with dementia evaluations underscores the meticulous approach required in patient care.
The interplay between existing medications and treatment eligibility further complicates the landscape, potentially limiting access for certain individuals. The protracted timeline to consult a neurologist adds another layer of complexity, exacerbating the delay in treatment initiation.
Despite the arduous path to treatment, patients like Berkheiser and Charles “Bum” Clegg exemplify resilience in their journey.
The meticulous balancing act between treatment sessions and daily commitments underscores the determination of individuals grappling with Alzheimer’s disease.
The testimonials of improved memory and renewed hope offered by patients and their families underscore the transformative impact of medical interventions in enhancing quality of life.
Looking ahead, prospects for improved treatment access offer a glimmer of hope for individuals affected by Alzheimer’s disease.
Ongoing research on alternative treatments such as Eli Lilly and Co.’s donanemab and Eisai’s injectable version of Leqembi herald a promising future. The potential for blood tests to expedite amyloid detection signifies a paradigm shift in diagnostic approaches.
However, the road ahead remains fraught with challenges, as the multifaceted nature of Alzheimer’s disease necessitates a holistic understanding and innovative treatment strategies.
In conclusion, the narrative of Alzheimer’s disease treatment access underscores the intricate interplay between healthcare systems, patient care, and medical advancements.
While progress in treatment accessibility offers hope for individuals like Berkheiser and Clegg, the journey towards combating Alzheimer’s disease remains a formidable task.
As Dr. Eric Widera aptly notes, the complexity of Alzheimer’s disease transcends amyloid pathology, necessitating a comprehensive approach towards unraveling its mysteries.
Only through concerted efforts in research, healthcare delivery, and patient advocacy can we pave the way towards a brighter future for those impacted by Alzheimer’s disease.

